Our ambition is for all pregnant FNP smoking clients to quit
Amy Williams, FNP National Unit Project Manager
Building quality improvement capacity in the Family Nurse Partnership National Unit is part of our strategy to ensure continuous improvement in the FNP programme in England through the applied use of quality improvement methodology. Our first port of call, using this methodology, has been to tackle smoking cessation. In July 2019, we completed the first phase of the FNP smoking cessation improvement project.
Smoking cessation remains a key priority for public health improvement work at both national and local level. The NHS Long Term Plan calls out smoking as a habit which “accounts for more years of life lost than any other modifiable risk factor.” It acknowledges the risks of smoking in pregnancy in particular, noting that an estimated one in four women smoke at some time during pregnancy in England.
Public Health England data suggests that teenage mothers are twice as likely to smoke before and during pregnancy, and three times more likely to smoke throughout pregnancy. This trend is partly reflected in FNP programme data, though we have seen a reduction in smoking during pregnancy among FNP clients, with around 23% of young mums on the programme saying they smoke at 36 weeks in pregnancy – the lowest prevalence for three years.
Despite this encouraging direction of travel, we are committed to going further: our ambition is for all pregnant FNP clients to quit smoking.
I have a vested interest in this work as an ex-smoker. It’s well known that people smoke for a variety of reasons, one of those being as a way to relieve stress and relax. I smoked during a particularly stressful time in my life, and it wasn’t until I had support that I was able to make the best decision for me and quit.
Like all public health professionals, family nurses have the power to make every contact count and that’s particularly relevant for our efforts to help young pregnant mums-to-be quit smoking. It’s a critical part of our role as a national unit, with strategic oversight of the FNP programme in England, to prove – with evidence – how that is happening on the ground and on what scale.
Quality improvement methodology advocates the use of continuous data. In practice, this means collecting data and monitoring it frequently enough to detect statistically significant changes in outcomes. We are using carbon monoxide monitors in our project to improve quit smoking rates among FNP clients in pregnancy. All family nurses in the five FNP teams we’re working with take a carbon monoxide reading during every visit with a pregnant client (smoking or not). Data is entered into the FNP data system.
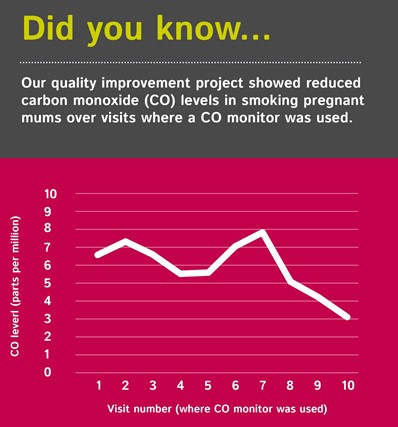
What we have seen in the data so far is encouraging. With an increased focus on smoking cessation during visits with pregnant clients, the average carbon monoxide level readings have decreased (across all clients in all five sites during visits where a monitor is used). It seems, so far, that the more a nurse increases focus on smoking cessation, the more likely it is that the client, over time, will reduce how much they smoke – and will ultimately quit.
We’ve focused specifically on the pregnancy stage in the FNP programme in light of the quality improvement principle of ‘starting small’. Our ambition is share learning across the FNP community. We want to move on to understanding what works in the infancy and toddler stages of the FNP programme, and we want to understand what it takes to help FNP clients achieve a sustained quit. Quality improvement gives us the structure and rigour to do this work, but the skill and dedication of our family nurses is key to achieving good outcomes for our clients.
We’re really grateful to all the family nurses, supervisors and quality support officers in the five FNP teams involved in the project for their commitment to this work. We hope the green shoots from this quality improvement project will take us one step further towards our ultimate ambition of seeing all pregnant FNP clients quit smoking.
